by Shelly Prosko, PT, PYT, CPI
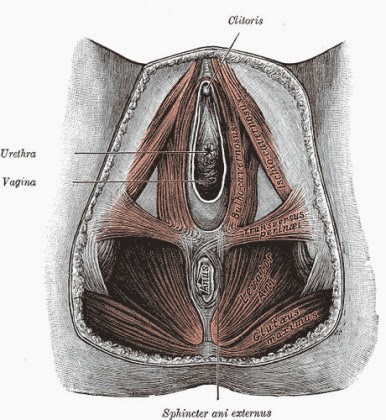 |
| Female Pelvic Floor Muscles
You sneeze or laugh and you accidentally “leak” a small amount of urine. You are embarrassed, but not concerned enough to seek treatment because, after all, this is a normal experience as we age, right? Wrong. It is true that urinary leakage is extremely common, but it is not normal. In fact, over 1/3 of men and women between the ages of 30-70 years old experience urinary incontinence (the inability to control the bladder) at some point in their lives. The prevalence is much higher in women than in men. However, it is estimated that 66% of us don’t even discuss it with our physicians! Perhaps this is because we don’t know there is help or because we are too embarrassed. For us women, maybe we believe that it is normal after childbirth and will eventually resolve. Perhaps we believe it is just another “normal process of aging.” But it is not a normal aging process. Urinary incontinence is a symptom of an underlying problem, and it can be prevented and treated in most cases! The two main types of urinary incontinence are stress and urge. In order to treat it properly, it is important to know the difference between the two, and to know which one you may have. However, it is common to have a combination of the two as well. Stress incontinence is what occurs when the pelvic floor muscles (PFM’s) have become too weak to stop the flow of urine during actions that put pressure or stress on the bladder, such as coughing, sneezing, laughing, twisting, or lifting. Pelvic floor weakness can result from the muscles being overstretched or damaged during trauma such as surgery or childbirth, or even from low estrogen levels, such as during menstruation or menopause. Additionally, the ability of any muscle to perform optimally depends partly on its length-tension relationship, which can be influenced by alignment. PFM activation could therefore potentially be compromised mechanically if postural alignment is suboptimal. Urge incontinence is when you have a sudden urge to urinate with an inability to control the bladder. This happens when the pelvic floor muscles are chronically tense to the point of fatigue, and consequently give out at inappropriate times. Chronically tense and tight PFM’s can be a result of an over-active bladder (OAB) where one experiences urinary urgency (urge to urinate) and/or frequency (urinating more frequently than normal). If your PFM’s are consistently tense, and you don’t know how to relax, release, and control them, other problems in addition to urge incontinence can arise, such as low back pain, irritable bowel syndrome, interstitial cystitis, bladder pain syndrome and painful intercourse. Many people believe that the popular Kegel exercises, which consist of “squeezing” the PFM’s, will solve all leakage problems. However, this is not necessarily the case! In order to truly have a healthy pelvic floor that functions optimally, you must first cultivate a sense of awareness of the area, and then learn how to release, engage and control. If your incontinence is partially due to chronically tensed PFM’s that are fatigued when you need them most (remember, even if your PFM’s are weak, they can still be tight!), then simply performing Kegel exercises may actually be worsening your problem! Starting by learning how to release your PFM’s in conjunction with a yoga breath, such as abdomino-diaphragmatic breathing: |
If your incontinence is PFM weakness due to being overstretched or inadequately activated, then correctly prescribed PFM exercises can help. In a later post, I will discuss the yoga principle of mula bandha, and how it might be used in treatment of incontinence. I do want to point out that I am by no means a bandha expert! However, much of my training and studying (from well respected yogis) has taught me that mula bandha is NOT simply activation of PFM’s. Also, keep in mind that the PFM’s are still only a small part of the overall treatment of this dysfunction.
If you don’t know which of these two PFM problems is causing your incontinence, I recommend consulting a qualified PT or other medical expert who specializes in pelvic health to help you figure out which type of incontinence you have.
Research has shown that successful physical therapy treatment of incontinence consists of protocols that also include hip adductor and deep abdominal muscle strengthening, lumbar or core stability training, and prescription of exercises that address postural misalignment or hip tightness that may be contributing to pelvic floor weakness.
As a physical therapist and yoga therapist, it has been extremely valuable to use yoga as part of therapy for incontinence issues. I have found that focused meditations such as body scanning and breath awareness have been instrumental in creating a higher awareness of the pelvic floor, which is the first step to releasing then engaging and controlling the PFM’s.
I recommend starting with what I call the “Toilet Meditation,” which is simply being completely present and aware when performing your toilet duties! Focus on observing the rhythm of both the respiratory AND the pelvic diaphragms as you breathe, releasing your PFM’s and taking your time. We often are rushing when we urinate, and may not even be fully emptying our bladders in the first place. If you suffer from mild leakage, you may be subconsciously tensing your PFM’s for fear of leakage throughout the day. That low grade tensing may carry over to when you are actually supposed to be relaxed, during urination. This can further create more tension and tightness in the PFM’s and potentially result in a sense of urgency to urinate throughout the day.
All this can lead to changes in your nervous system. Messages from your bladder to your brain become hypersensitive, and the part of the nervous system that sends the message “hurry hurry, I have to go” overrides the part of the nervous system that sends the message “no, it’s okay, chill, we got time—the bladder has much more room yet.” This can also lead to behavioral changes. For example, as you read this, are you feeling an uncomfortable urge to urinate? Or if you hear running water, does it increase your urge?
Anecdotally, I have seen a number of women whose incontinence issues started with mild stress incontinence that developed into more severe urge incontinence. Therefore, it has led me on a path to be a huge advocate for teaching pelvic floor awareness and release first, before simply teaching contract and squeeze methods. This is one major advantage that yoga, or any mind-body practice, can have in treating incontinence more than just a traditional western medicine approach alone.
I also have found that the abdomino-diaphragmatic breath or belly breath, with awareness of the natural motion of both the diaphragms, has been a great tool to begin addressing incontinence. Some of my favorite yoga poses in which to perform and observe this breath are: Crocodile pose (Makarasana), Garland pose (Malasana), Extend Child’s pose (Balasana), Hero pose (Virasana), and Reclined Cobbler’s pose (Supta Baddha Konasana).
In my next post, I will focus on how yoga can more specifically address incontinence issues. Remember, although incontinence is common, it can be treated. So whether you are a new mom or a retiree, you can still continue to enjoy a healthy lifestyle knowing you have confidence in controlling your bladder!
Follow Yoga for Healthy Aging on Facebook ° To order Yoga for Healthy Aging: A Guide to Lifelong Well-Being, go to Amazon, Shambhala, Indie Bound or your local bookstore.

Shelly, I cannot begin to express my gratitude for you broaching this subject! Already so much of what you say resonates. Excited to learn more! Thank you
I'm so grateful that you appreciate this information! I find that there is a large amount of inaccurate information out there regarding this subject. Sharing and offering as much as I can about pelvic health is something I'm very passionate about!
Way back in the day "shields" and "guards" had more rugged meanings.
Great article! Look forward to more information on this important subject .
Good tips. I don't think you are far off the mark when you say that people sometimes rush.
Interesting! You mention about becoming 'present and aware' during toileting. Toilet meditation is a good idea. In teaching the Mula Bandha I encourage people to practice right there on the toilet. Stopping flow and then 'releasing and relaxing' to encourage flow. Doing this several times, like 'reps' is the way to really learn to understand the feeling of Mula Bandha. 'Steady and Comfortable' are the principles to employ. A steady and comfortable hold. Releasing while exhaling is essential as well. Combining the breath in this way trains the parasympathetic system to connect with the conscious awareness. Setting the Mula Bandha or engaging the 'holding aspect' ie, stopping the flow, should also be done at the end of an exhalation. When we inadvertently release the Root Lock or Mula Bandha during a mat or asana practice there is either too little or too much tension, awareness or intensity in the pose itself. The trick of course is to find the balance between all of the elements. I always look eventually for the still place where the inbreath ends and the outbreath begins as my centre to observe all of these aspects from. Great article, insightful and packed with info. These issues do become something people are more prone to as they age, have babies or simply from over stretching….so it's important to be able to discuss this matter intelligently, with a proactive and positive approach such as this article so aptly does.